Imagine a world where damaged brain cells can be replaced—not just treated, but regrown. That’s no longer science fiction. A group of pioneering Japanese scientists has made history by developing a revolutionary therapy for Parkinson’s disease using lab-grown brain cells. This innovation could redefine how we approach neurodegenerative diseases—and it’s already showing stunning results.
Let’s dive into what this breakthrough means, how it works, and why it’s giving new hope to millions around the world.
Understanding Parkinson’s Disease: The Basics
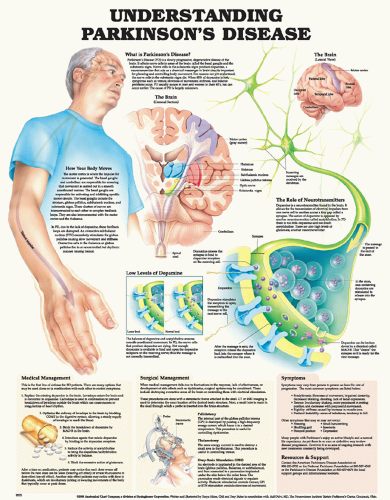
Parkinson’s disease is a progressive neurological disorder that primarily affects movement. It happens when dopamine-producing neurons in a specific part of the brain—called the substantia nigra—begin to die off. Dopamine is the chemical that helps control motor function, and when it’s in short supply, symptoms like tremors, stiffness, and slowness take over.
Current treatments, like medications (Levodopa) and deep brain stimulation, only manage the symptoms. They don’t address the core issue: the loss of dopamine-producing neurons.
But what if we could actually replace those missing brain cells?
The Stem Cell Solution: How It Works
Here’s where Japanese researchers flipped the script. They used induced pluripotent stem cells (or iPS cells)—adult cells reprogrammed to return to a stem cell-like state. From there, they guided these iPS cells to develop into dopamine-producing neurons. These are the exact types of cells that deteriorate in Parkinson’s patients.
The process goes like this:
- Scientists take skin or blood cells from a donor.
- They reprogram those cells into iPS cells.
- The iPS cells are then matured into dopamine neurons.
- These lab-grown neurons are implanted directly into the brain of a Parkinson’s patient.
Video : Japanese Scientists Announce New Tests On ‘Reprogrammed’ Stem Cells In Treating Parkinson’s Disease
Early Results Are In—And They’re Promising
So far, a handful of patients have undergone the procedure. The outcomes?
- Improved movement control within months of the transplant.
- Brain scans confirm dopamine production by the implanted neurons.
- No signs of rejection or dangerous side effects reported during the monitored trial period.
One patient reportedly reduced their reliance on Parkinson’s medications by nearly 50% post-implantation. While it’s still early, the data suggests that these new neurons are doing more than surviving—they’re thriving.
Why This Breakthrough Is Such a Big Deal
To understand the scale of this innovation, let’s break down its major implications:
1. It Targets the Root Cause
Unlike current treatments that treat symptoms, this therapy replaces the exact neurons Parkinson’s disease destroys. That’s not just treatment—it’s regeneration.
2. It Uses the Patient’s Own Cells
Because iPS cells can be derived from the patient themselves, the risk of immune rejection is drastically reduced. It’s personalized medicine in its most powerful form.
3. It Could Extend to Other Brain Diseases
While the focus is Parkinson’s right now, the technology behind iPS cells could be adapted to treat:
- Alzheimer’s disease
- Huntington’s disease
- ALS (Lou Gehrig’s disease)
- Stroke damage
The door is now open to a whole new category of regenerative neurology.
From Lab Bench to Hospital Bed: What’s Next?

Although early trials are exciting, there’s still a journey ahead before this therapy becomes standard.
More Clinical Trials: Larger groups and longer follow-ups are needed to fully understand safety, long-term effects, and ideal conditions for implantation.
Production Scaling: Creating lab-grown neurons is complex and expensive. Scientists are now working on streamlining the process for broader use.
Ethical Oversight: As with any advanced medical technology, strict guidelines are needed to ensure responsible and ethical use.
Japan has already approved early-stage human trials, and if future results continue to impress, we could see fast-tracked approvals in Europe and North America.
What This Means for Patients Around the World
For over 10 million people globally living with Parkinson’s, the message is simple: there’s hope. This isn’t just a better drug—it’s a potential cure at the cellular level. And it’s happening in our lifetime.
Imagine a world where:
- A Parkinson’s diagnosis doesn’t mean permanent decline.
- Brain damage isn’t the end, but a starting point for regeneration.
- A simple surgery could restore years of lost movement and independence.
This is the promise of stem cell medicine—and we’re closer than ever to making it real.
Japan: Leading the Charge in Regenerative Neuroscience
Japan has long been a leader in cutting-edge biomedical research, especially in the stem cell space. The Nobel Prize-winning scientist Shinya Yamanaka, who first discovered iPS cells, laid the groundwork for this very breakthrough.
Video : Parkinson’s patient moves freely again after world-first implant of lab-grown cells into his brain
Now, Japanese hospitals and research institutions are turning discovery into treatment. They’ve built a clear regulatory path to allow carefully monitored trials while prioritizing patient safety.
Their progress could become a global blueprint.
Final Thoughts: The Future of Healing Is Here
Every so often, a scientific discovery comes along that changes everything. This is one of those moments.
By using iPS cells to regrow dopamine-producing neurons and successfully implanting them into patients, Japanese scientists have opened a new chapter in the fight against Parkinson’s disease. It’s no longer just about slowing decline—it’s about reversing it.
We’re not just managing symptoms anymore. We’re talking about rebuilding the human brain.
The road ahead will still have hurdles, but one thing is clear: regenerative medicine isn’t coming—it’s here.
Would you consider stem cell therapy if it became available for a loved one with Parkinson’s? Let’s talk about it in the comments below. And don’t forget to share this article with someone who could use a little hope today.