In a time where cancer prevention has become smarter and more proactive, a new study has delivered a surprising—and deeply concerning—reality check. Anal cancer cases are on the rise, and the most vulnerable group may not be who you expect. According to fresh research presented at Digestive Disease Week, older women, particularly those over 65, are experiencing the fastest-growing rates of anal cancer in the United States.
Let’s unpack the findings, understand why this shift is happening, and explore what can be done to protect the health of aging women.
Understanding Anal Cancer: The Basics
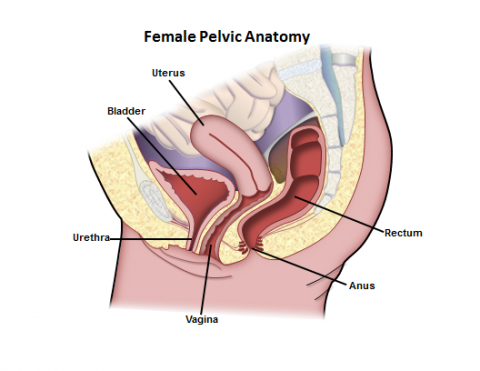
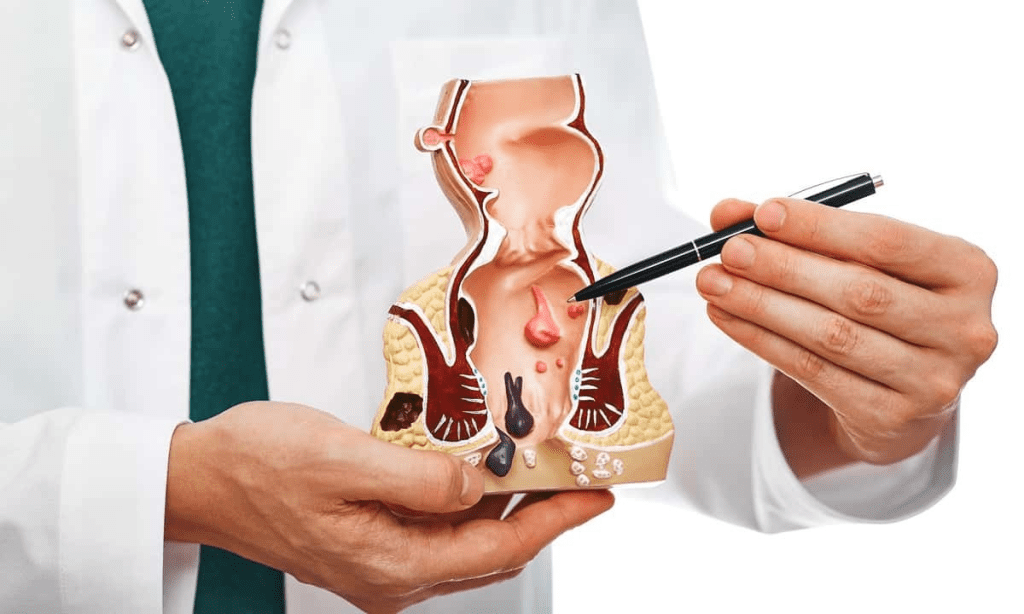
Anal cancer starts in the anal canal, the short passage at the end of the rectum. It’s not commonly talked about—and for many, it’s still shrouded in stigma. But this silence can be dangerous. Symptoms such as bleeding, pain, itching, or the presence of a lump are often mistaken for less serious issues like hemorrhoids. That delay in diagnosis can cost precious time.
The latest data from the U.S. National Cancer Institute between 2017 and 2021 show that anal cancer isn’t just increasing—it’s gaining momentum, particularly in older women. So why now?
Older Women Are Facing the Highest Risk
The study revealed a clear and troubling pattern: white and Hispanic women over 65 saw the steepest increases in anal cancer diagnoses. For women over 65, the annual rise was 4.3%. Hispanic women in this same age group experienced a 1.7% annual increase.
What’s driving this surge?
One likely factor is limited access to or uptake of the HPV vaccine. Human papillomavirus (HPV) is responsible for the vast majority of anal cancer cases, but many women in this age group missed out on vaccination. After all, the vaccine was only introduced in 2006—and by then, many women now in their 60s or 70s were well beyond the target age range.
Video : Anal Cancer Facts: What Causes It and How to Fight It
The HPV Connection: A Hidden Risk
HPV is an extremely common virus, spread primarily through sexual contact. While most HPV infections clear on their own, some strains can linger and cause cancers—including cervical, oral, penile, and anal cancers.
The CDC recommends HPV vaccination for everyone through age 26 and, in some cases, up to age 45. In the UK, children as young as 12 are routinely offered the vaccine.
But back when today’s 65+ women were younger, this kind of prevention didn’t exist. They may have carried HPV for decades without ever knowing it. This silent exposure may now be translating into late-onset anal cancer cases.
Why Are Symptoms Often Missed?
One reason this rise is particularly dangerous is because anal cancer symptoms are subtle—and easily brushed off. A bit of bleeding or discomfort during bowel movements? Many assume it’s just hemorrhoids or aging. That hesitation to speak up or seek help can delay diagnosis.
Dr. Ashley Robinson, the study’s lead author, emphasized how essential awareness is. “We’re seeing a population that was never considered high risk now facing a clear uptick in cases,” she said. “We need to talk about this more.”
Screening Gaps: A Missed Opportunity
Currently, there is no routine screening for anal cancer in older women. Unlike cervical cancer, which benefits from regular Pap smears, anal cancer is often detected late—when treatment is more difficult.
This study suggests it may be time to rethink that approach. If older women are now showing increased risk, especially due to past HPV exposure, shouldn’t they be offered tailored screening options?
Just as we adapted breast cancer screening to better serve women over 50, it may be time for a similar update for anal cancer.
Vaccination: Still Relevant Beyond Adolescence
Many adults assume that HPV vaccination is just for teens. But that’s changing. The FDA has approved the vaccine for people up to age 45. While it won’t eliminate pre-existing infections, it can still provide protection against other strains and future complications.
If you’re an adult who missed the window for HPV vaccination in your youth, talk to your doctor. It might not be too late to protect yourself.
What Can Older Women Do Right Now?
Knowledge is power, especially when it comes to your health. If you’re over 60—or you have a loved one in this age group—here’s what you can do today:
- Know the symptoms. If you notice unusual anal bleeding, persistent itching, or a lump, don’t ignore it. See a healthcare provider promptly.
- Ask about HPV vaccination. If you’re under 45 and haven’t been vaccinated, it’s worth asking your doctor if you’re eligible.
- Talk about screening. While anal cancer screening isn’t routine, you can advocate for yourself. If you’re at higher risk, such as a history of HPV-related disease, ask if screening makes sense for you.
- Don’t assume you’re not at risk. Cancer doesn’t follow assumptions or stereotypes. This study proves that risk profiles can change—and when they do, so should our health strategies..
Video : I Want Everybody To Know: A HPV Anal Cancer Survivor Story
The Bigger Picture: Let’s Break the Silence
Anal cancer isn’t often part of mainstream health conversations. But maybe it should be. When the numbers start rising—especially in a vulnerable population—we owe it to ourselves and our communities to talk about it.
Awareness, prevention, and smart screening guidelines can save lives. And that starts with shedding the stigma and embracing open, honest discussion.
Conclusion: Prevention Starts with Awareness
The recent rise in anal cancer cases among older women is more than a medical trend—it’s a wake-up call. It reminds us that the effects of past exposures, such as HPV, don’t always appear right away. It also highlights the need to update our health strategies to match today’s risks, not yesterday’s assumptions.
If you or someone you love is in that 65+ age group, now is the time to ask questions, stay informed, and take proactive steps toward protection. Because when it comes to cancer, early awareness is everything—and it just might save your life.


