Understanding Peptic Ulcer Disease
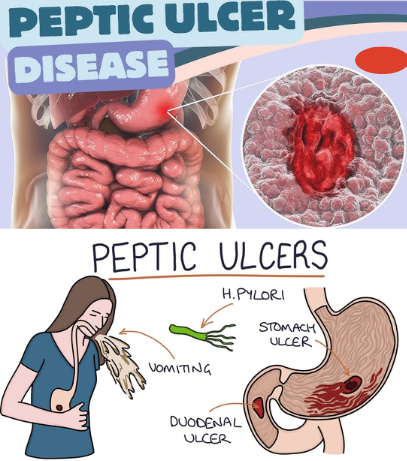
Have you ever felt a burning pain in your stomach that just won’t go away? That discomfort could be more than simple indigestion—it might be a peptic ulcer. A peptic ulcer is an open sore that develops in the lining of the stomach (gastric ulcer) or the upper part of the small intestine (duodenal ulcer). These ulcers form when the protective lining of the digestive tract is weakened, allowing stomach acid to cause damage. While they can be painful, peptic ulcers are highly treatable once diagnosed.
What Causes Peptic Ulcers?
Contrary to popular belief, ulcers aren’t caused by stress or spicy foods alone. The two main culprits are:
- Helicobacter pylori (H. pylori) infection – A bacteria that weakens the stomach lining, making it more vulnerable to acid.
- Long-term use of NSAIDs – Pain relievers like ibuprofen and aspirin irritate the stomach lining over time.
Other contributing factors include:
- Excessive alcohol consumption
- Smoking
- High levels of stress (which worsen symptoms)
- Genetic predisposition
- Other serious illnesses that increase stomach acid production
Think of your stomach lining as a shield. When bacteria or medications weaken it, stomach acid slips through and creates painful sores.
Recognizing the Symptoms
Peptic ulcer symptoms can vary, but the most common signs include:
- Burning stomach pain, especially between meals or at night
- Bloating and belching
- Nausea or vomiting
- Loss of appetite or unintentional weight loss
- Dark or tarry stools (a sign of bleeding)
- Fatigue from anemia if blood loss occurs
The pain may come and go but usually follows a pattern—getting worse on an empty stomach and improving temporarily after eating.
Video : Gastritis and Peptic Ulcer Disease (PUD) – Medical-Surgical (Med-Surg) – Gastrointestinal System
How Peptic Ulcers Are Diagnosed
If you suspect you have an ulcer, a doctor will use a combination of methods to confirm:
- Medical history and symptoms review – First step to identify possible triggers.
- Endoscopy – A camera tube is inserted to directly view the ulcer.
- H. pylori test – Can be done via breath, stool, or biopsy samples.
- Imaging scans – In severe cases, X-rays or CT scans check for complications like perforation.
An accurate diagnosis ensures that the right treatment plan is followed.
Treatment Options for Peptic Ulcers
The good news? Most ulcers heal with proper care. Treatments include:
- Antibiotics – If H. pylori is present, a course of antibiotics is prescribed.
- Proton pump inhibitors (PPIs) – Reduce acid production, giving ulcers time to heal.
- H2 blockers – Another class of drugs that lower acid levels.
- Antacids – Provide quick but temporary relief.
- Protective medications – Coating agents like sucralfate protect the stomach lining.
- Lifestyle adjustments – Avoiding alcohol, NSAIDs, and smoking speeds up recovery.
Severe ulcers that bleed, perforate, or don’t heal with medication may require surgery.
Complications if Left Untreated
Ignoring peptic ulcers can lead to dangerous complications, such as:
- Internal bleeding – Leading to anemia or black stools.
- Perforation – A hole in the stomach or intestine wall causing severe infection.
- Obstruction – Swelling or scarring that blocks food passage.
- Increased cancer risk – In rare cases, chronic ulcers caused by H. pylori may increase stomach cancer risk.
That’s why early detection and treatment are vital.
How to Prevent Peptic Ulcers
Prevention is always better than treatment. Here are simple habits to protect your stomach:
- Wash hands often and eat clean food to reduce H. pylori risk.
- Limit long-term use of NSAIDs or take them with protective medications.
- Reduce alcohol and quit smoking to improve healing.
- Eat smaller, balanced meals and avoid late-night heavy snacks.
- Manage stress with relaxation techniques like meditation or yoga.
Think of prevention as building a stronger shield around your stomach lining.
Lifestyle Tips for Better Digestive Health
If you’ve had ulcers before or are at risk, daily choices can make a difference:
- Stay hydrated—water dilutes stomach acid.
- Include probiotics in your diet—yogurt and fermented foods help restore gut balance.
- Choose anti-inflammatory foods—leafy greens, berries, and omega-3s.
- Avoid overly spicy or acidic foods if they worsen symptoms.
- Get regular check-ups if you’ve had ulcers in the past.
Consistency is key. Your digestive system thrives when treated gently and supported with healthy choices.
Video : Your guide to peptic ulcer disease
Conclusion
Peptic ulcer disease is common but far from unbeatable. By understanding the causes, recognizing early symptoms, and adopting both medical and lifestyle solutions, you can prevent complications and enjoy better digestive health. Whether caused by H. pylori, medications, or lifestyle factors, ulcers can heal with the right care. Remember: your stomach is resilient—give it the support it needs, and it will repair itself over time.


